Heart attack awareness in Australian masters football players
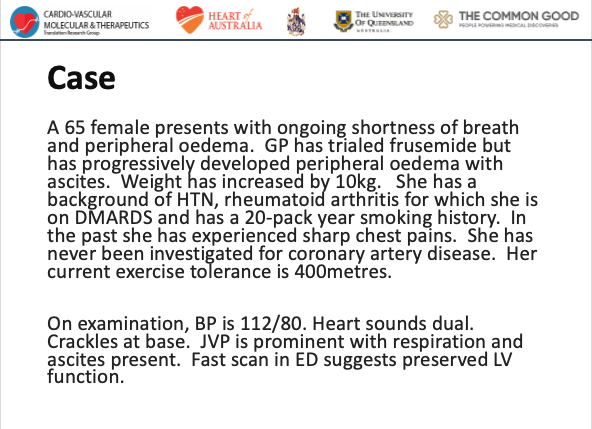
A half of over-35s are not confident in their ability to recognise symptoms of impending cardiac risk – such as a heart attack or sudden cardiac death – while participating in strenuous exercise. A paper published today in The Internal Medicine Journal surveyed 153 Masters Age football players aged ≥35 years playing on a scale of competitive to social football games.
Participants exercised or played sport an average of 3.6 days per week, with a weekly average of 2.6 hours of moderate activity and 2.4 hours of vigorous activity.
Professor Geoffrey Tofler, senior author of the paper and of University of Sydney and Royal North Shore Hospital, says, “Although regular exercise improves health, strenuous exercise causes a transient increase in cardiac risk. Being able to recognise the warning signs of an impending cardiac event is critical to mitigating those risks during exercise.”
“The risks are elevated when accounting for participants with pre-existing risk factors like hypercholesterolaemia, hypertension, smoker status, weight issues, and family history of heart disease.”
Despite the popularity of Masters football, the prevalence of cardiac risk factors and
potential cardiac symptoms in players has not been adequately studied.
“In total, one in five study participants had one or more possible cardiac symptoms during a game in the prior year, but only a quarter of them sought medical attention.
In a hypothetical scenario of participants having chest pain while playing, around half of them said they would keep playing for five to ten minutes waiting for the symptoms to pass.”
“Almost half of the participants were unsure whether they would recognise symptoms they might experience during games, such as chest pain, as an indicator of potentially serious cardiac risk.”
The need for better cardiac education and knowledge has been emphasised as a key solution to preventing or mitigating cardiac events. Most of the cohort surveyed agreed that external defibrillators and CPR training were important and should be staples at football fields during all games.
“Performing CPR and using a defibrillator could be the line between life and death for someone experiencing sudden cardiac arrest, as the survival rate decreases by seven to ten per cent for every minute without the use of either method.” says Professor Tofler.
“Education strategies should focus on giving players clear instructions to assist rapid symptom recognition and management of cardiac events.”
“While it is important to note that the benefits of exercise still far outweigh cardiac risk overall, these measures may further increase the benefit to risk ratio.”
Key Findings
Out of the 153 participants:
50% were not confident in their ability to recognise symptoms of a heart attack in themselves with even less (33%) expressing confidence in recognising one in others.
1 in 5 participants reported experiencing one or more potential cardiac symptom during physical activity in the preceding 12 months.
Only 24% (one quarter) of those experiencing one or more symptoms sought medical attention
In a hypothetical scenario of a participant experiencing chest pain while playing
47% said they would leave the field immediately however 49% would continue playing for 5-10 minutes to see if the pain eased, and several would continue playing further.
One third would be embarrassed to go to hospital if they thought they were having a heart attack but were incorrect
45% said that if they thought they were having a heart attack, they would rather someone drive them to hospital that have an ambulance come to their home”
Only 40% were aware that warning symptoms may precede a heart attack by days or more.
67% knew how to provide CPR