Pulmonary Hypertension in Mitral Regurgitation
Presented by Dr Seshika Ratwatte
Pulmonary hypertension (PHT) commonly co-exists with significant mitral regurgitation (MR), but its prevalence and prognostic importance has not been well documented. In MR, PHT is thought to be due to the direct effect of systolic backflow into the left atrium (LA), causing backpressure into the pulmonary vasculature and may develop before patients experience symptoms or left ventricular (LV) systolic dysfunction.
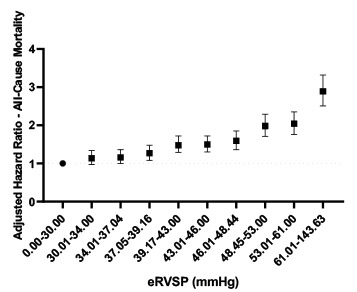
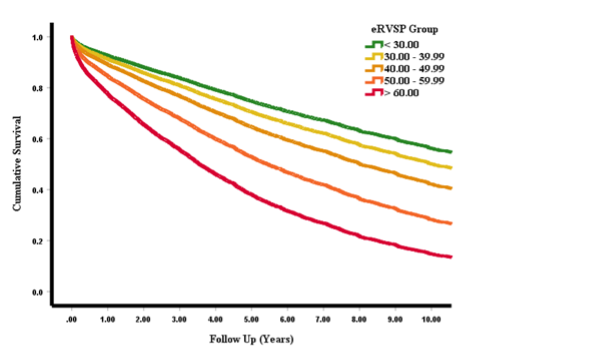
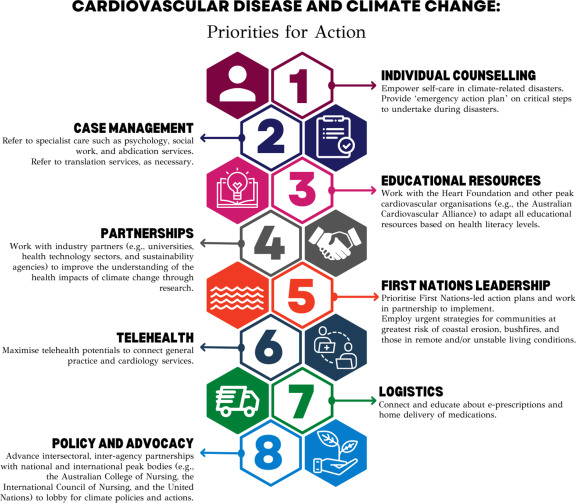
In an upcoming publication in Open Heart, Dr Seshika Ratwatte, senior author Professor David Celermajer and their co-authors identify a cohort of 9683 patients with “isolated” moderate or severe MR and preserved left ventricular ejection fraction (LVEF>50%) using the National Echo Database of Australia (NEDA). The authors show that the risk of all-cause mortality progressively increases as eRVSP level increases even after adjustment for age and sex, with an ‘inflection’ for mortality seen from eRVSP 34mmHg onwards (Central Illustration).
The publication confirms the high prevalence of PHT in patients with significant MR and preserved LVEF on echo (59.6%). Whilst a treatment effect was not reported, it was demonstrated that even minor elevations in pulmonary pressures were associated with negative prognostic implications. Consistent with the authors work on PHT in aortic regurgitation a typical phenotype of “left heart disease” on echo was confirmed the proportion of patients with RV dilation and functional impairments as well as right and left atrial sizes increasing progressively, from no PHT to severe PHT.
Central Illustration:
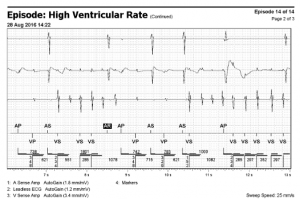
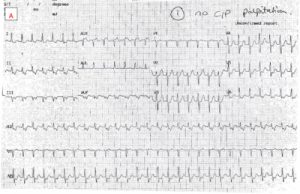
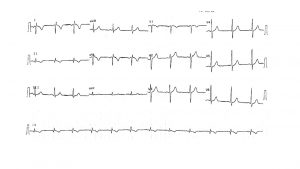
ECG of the Month, presented by A/Prof Alex Voskoboinik
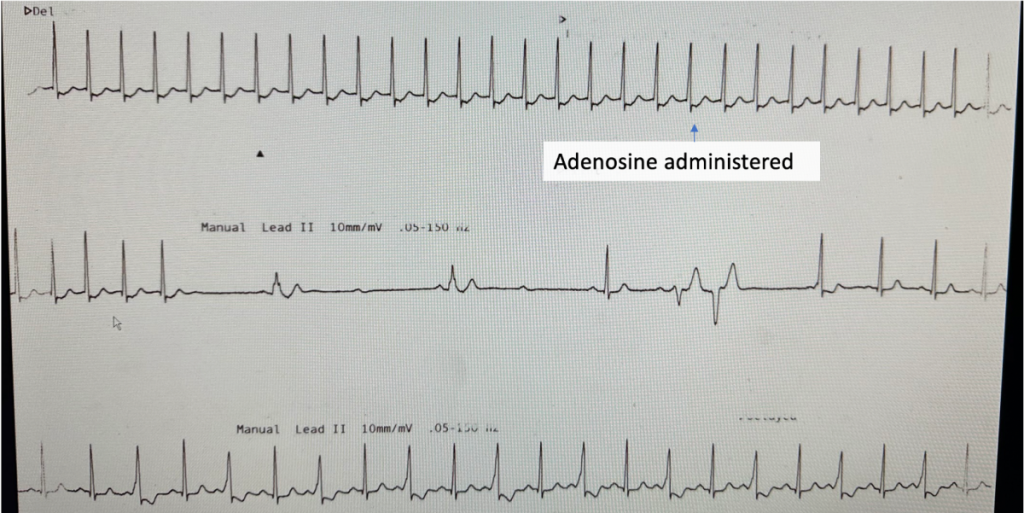
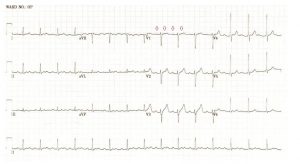
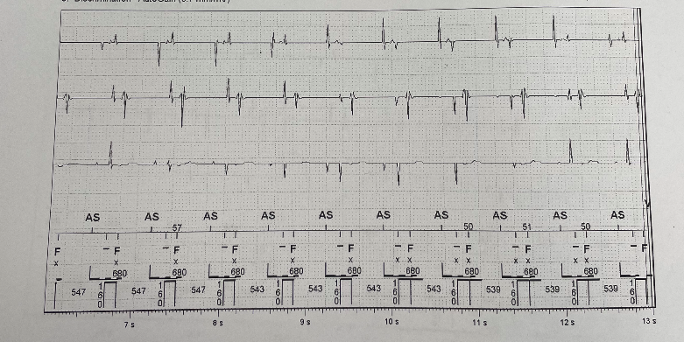
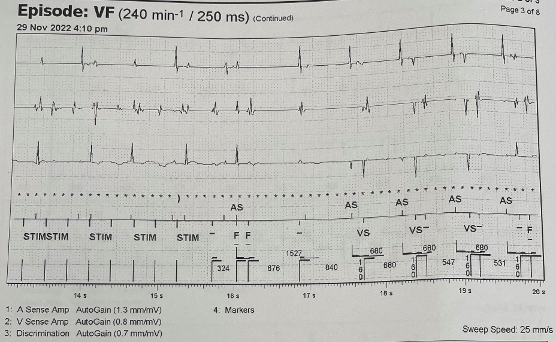
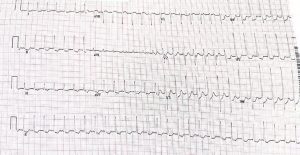
A 72 year old woman presents with palpitations and pre-syncope. Initial ECGs is shown below (Figure 1):
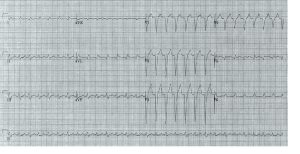
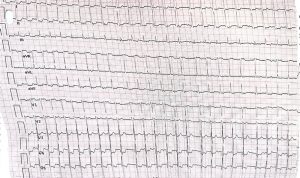
A Valsalva manoeuvre is attempted and subsequent ECG is shown below (Figure 2):
What is the most likely diagnosis? Want to ask a question or discuss visit the ECG Forum…
Answer:
Atrial tachycardia with Wenckebach AV nodal conduction.
Explanation:
The initial ECG demonstrates a ‘short RP’ SVT with the p-wave best seen in lead aVL on the initial ECG. The differentials are typical atrioventricular nodal reentrant tachycardia (usually the retrograde p wave is buried at the end of the QRS which is not the case here), atrioventricular reentrant tachycardia or atrial tachycardia (AT) with first degree AV block.
The second ECG following a ‘vagal’ manoeuvre does not terminate the tachycardia but increases the block at the level of the AV node. This exposes the p-waves and there are more ‘A’s than ‘V’s with grouped beating seen (best appreciated in lead III). This Wenckebach pattern excludes AVRT (in fact by definition the A:V relationship must be 1:1) and makes AVNRT very unlikely. The p-wave morphology is nearly isoelectric in V1 and very ‘skinny’ suggesting a mid-line origin. In pact at EP study the focal atrial tachycardia was mapped to the perinodal region and successfully ablated there.
Extensive pulmonary artery embolisation and pulmonary hypertension caused by cardiac hydatid cyst rupture
Extensive pulmonary artery embolisation and pulmonary hypertension caused by cardiac hydatid cyst rupture
Dr Jason Harmer
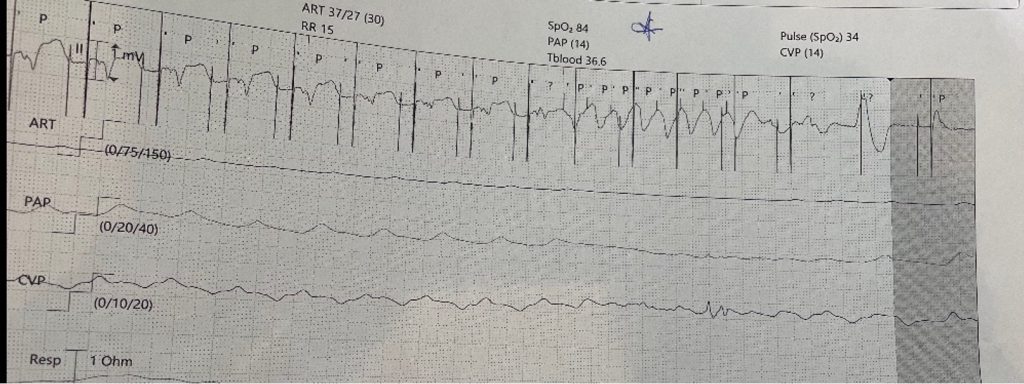
This case is a rare example of cardiac hydatidosis found in a patient in rural NSW, Australia. He was a middle-aged man who initially presented with a ruptured right ventricular hydatid cyst causing an anaphylactoid-like reaction, pulmonary emboli and widespread dissemination of hydatid echinococcus throughout the lung. He survived the cyst rupture and underwent cardiac surgery, but had incomplete resection and experienced progressive cardiopulmonary hydatidosis despite ongoing antihelminthic therapy. He had an array of cardiopulmonary sequelae over his lifespan, including worsening pulmonary hypertension and right heart failure, as well as bone marrow suppression and neutropenic sepsis. This case highlights rare clinical manifestations of cardiac hydatidosis and potential complications of its treatment.
Hydatidosis is caused by ingestion of larvae from the Echinococcus granulosus tapeworm from contaminated food or water supply or by direct contact with infected animals. Hydatid cysts commonly affect the liver or lung; however, cardiac involvement can occur in rare cases (i.e. <2% of all cases of hydatidosis).
Figure 1
Transthoracic echocardiogram: apical 4 chamber view. Intracardiac hydatid cyst.
Apical attachment of a large hydatid cyst to the wall of the RV. The RV chamber is dilated and hypokinetic and the septum is dyskinetic. The distal portion of the hydatid cyst is mobile. The RA is severely dilated and the interatrial septum is displaced due to pressure overload. The tricuspid annulus appears dilated.
Figure 2
Transthoracic echocardiogram: parasternal short axis view. Intracardiac hydatid cyst.
There is a large mass (hydatid cyst) in the RV that appears to be fixed to parts of the interventricular septum. Motion of the interventricular septum is abnormal, in part due to attachment of the mass and from raised pressures in the right heart. Interventricular septal flattening is a sign of raised right heart pressures. This patient has known moderate to severe pulmonary hypertension as a consequence of dissemination of hydatid disease to the lung and pulmonary thromboembolism.
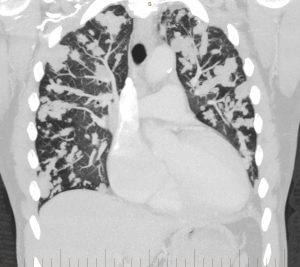
Figure 3
CT pulmonary angiogram: coronal view. Multiple hydatid masses within the pulmonary vasculature.
Multiple lobulated areas within the pulmonary vasculature from extensive dissemination of hydatid disease originating from the RV.
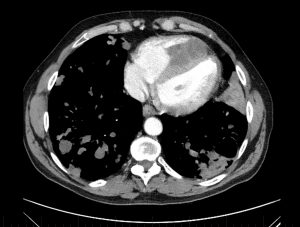
Figure 4
CT pulmonary angiogram: axial view.
There is a dense mass within the RV chamber due to a hydatid cyst. There is reduced RV blood filling in diastole due to the space occupying mass. The interventricular septal wall is clearly demarcated and the mass appears to encroach on the septal wall at two points. The RV is enlarged and occupies the apex of the heart. The sternum has been divided in two parts from a previous stenotomy (with incomplete surgical resection of the mass, leading to regrowth). There is a cavitating lesion in the posterior aspect of the left lung.
Abbrev. CT = computed tomography; RV = right ventricle; LV = left ventricle; RA = right atrium.
Pulmonary Hypertension in Aortic Regurgitation
Pulmonary Hypertension in Aortic Regurgitation
by Dr Seshika Ratwatte
Pulmonary hypertension (PHT) is known to complicate left heart diseases (LHD) including left sided valvular pathologies such as aortic regurgitation (AR). Patients with significant AR have an increased risk of death, even if they do not have symptoms, so identifying variables which predict adverse outcomes is important. PHT is thought to develop in AR due to left ventricular volume overload which eventually leads to increases in left atrial pressure and the development of post-capillary PHT.
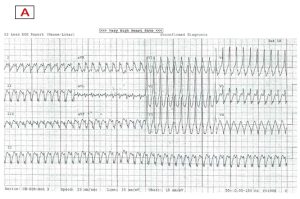
Now published in BMJ Heart, Dr Seshika Ratwatte, senior author Professor David Celermajer and their co-authors identify a cohort of 8392 patients with “isolated” moderate or severe AR and preserved left ventricular ejection fraction (LVEF>50%) using the National Echo Database of Australia (NEDA). The authors show that the risk of all-cause mortality increases as eRVSP level increases even after adjustment for age and sex (Central Illustration), with a ‘threshold’ for mortality seen from mild PHT onwards.
The publication outlines that a significant proportion of the population with significant AR had suspected PHT based on echo. Echo remains the first line screening tool to detect PHT and is the guideline recommended diagnostic method of choice to allow for monitoring and follow up. Clinicians need clear parameters to monitor and prognosticate such patients accurately. The authors identified a typical phenotype of “left heart disease” on echo with E:e’, right and left atrial sizes and the proportion of patients with RV functional impairments increasing progressively, from no PHT to severe PHT.
Central Illustration:
Link to publication is now available in BMJ Heart. https://heart.bmj.com/content/early/2023/04/02/heartjnl-2022-322187
Call for Papers – Heart, Lung and Circulation Special Issue: Cardio-Oncology
CALL FOR PAPERS Heart, Lung and Circulation Special Issue: Cardio-Oncology The 2023 Special edition of Heart, Lung and Circulation will examine the emerging discipline of cardio-oncology.
Download pdf and read more (pdf)